Background
About Cerebral Hemorrhage
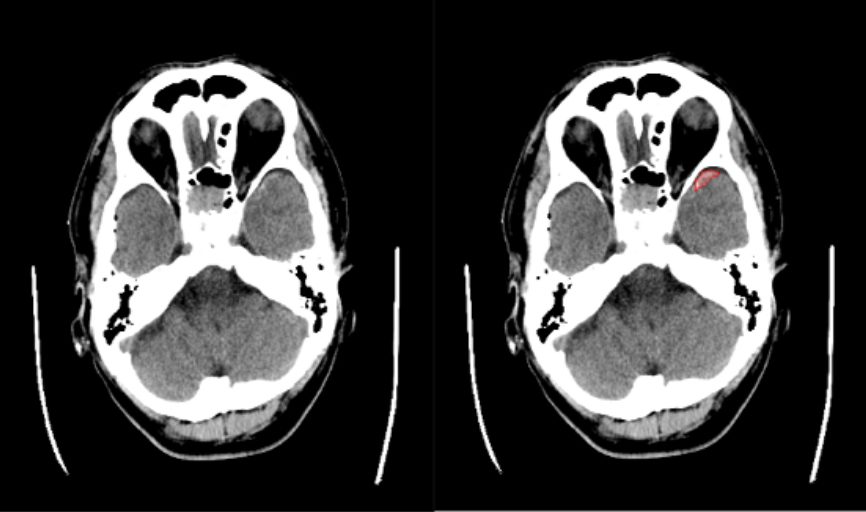
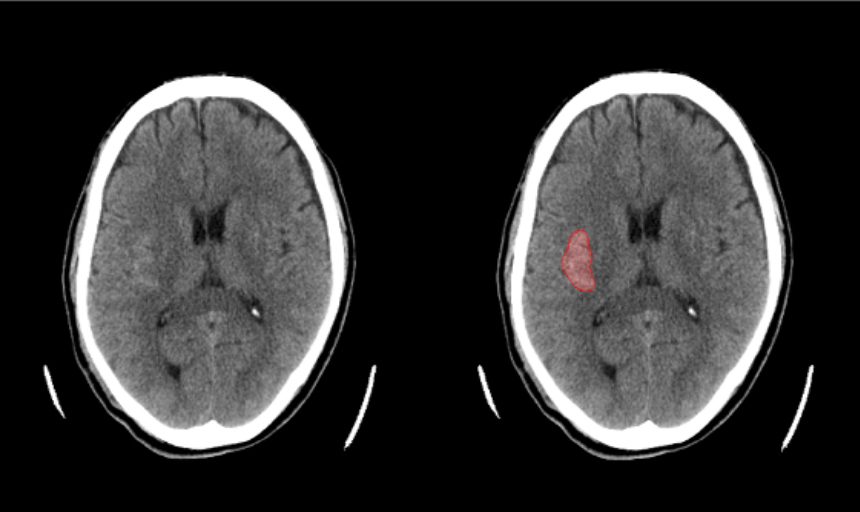
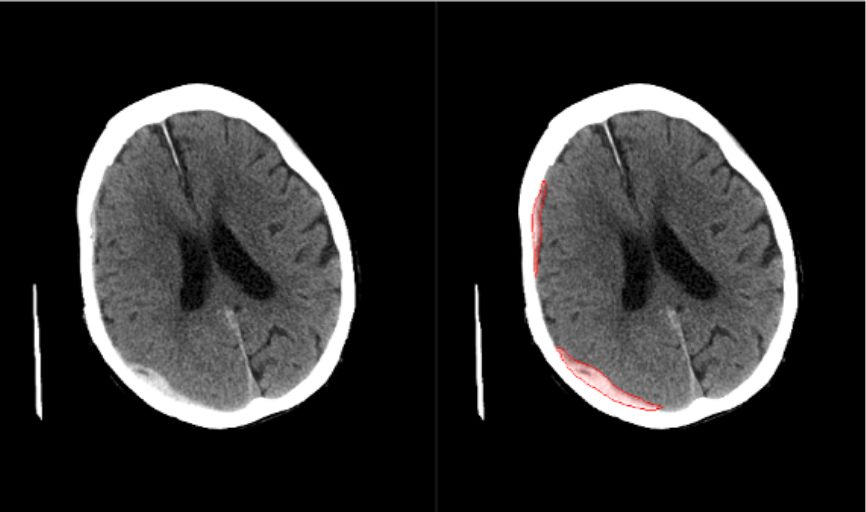
Cerebral hemorrhage, one of the most common types of strokes, is a condition in which a cerebral artery breaks and bleeds into the brain due to hypertension, brain tumors, or abnormalities in cerebral blood vessels. Nerve cells in the brain may be compressed by bleeding in various locations, causing symptoms such as headache, limbs paralysis, or loss of consciousness. When these symptoms are observed, a head CT scan is performed to determine the location and amount of bleeding from the findings of white-appearing areas (high attenuation areas) compared to the surrounding normal structures. Thus, a definitive diagnosis is made.
About Cerebral Hemorrhage and emergency medical care
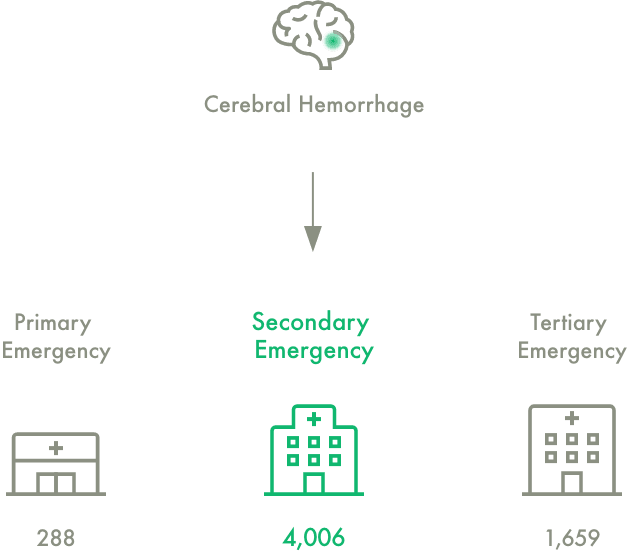
Depending on the severity of illness/injury and the urgency, patients are divided into three levels (primary, secondary, or tertiary) of emergency care. Patients categorized into the secondary emergency care are delivered to a medical facility, where doctors with extensive knowledge and experience in emergency medicine can provide inpatient care, including treatment and surgery, 24 hours a day.
As of October 2017, there are 4,006 facilities for secondary emergency care in Japan[1], and they are the most widely established.
For treatment of strokes such as cerebral hemorrhage, while tertiary emergency care facilities accept critically ill patients, secondary emergency care facilities have also played a significant role, treating 60% of such cases[2].
Accordingly, the following issues have become apparent.
Strengthening the system for secondary emergency care
Approximately 70% of hospitals have only one doctor in charge of on-call emergencies[3], and in some cases non-specialized doctors have to diagnose cerebral hemorrhage. This system may cause a risk of oversight, and there is a need to establish a better system in light of limited medical resources.
Reducing emergency department overuse
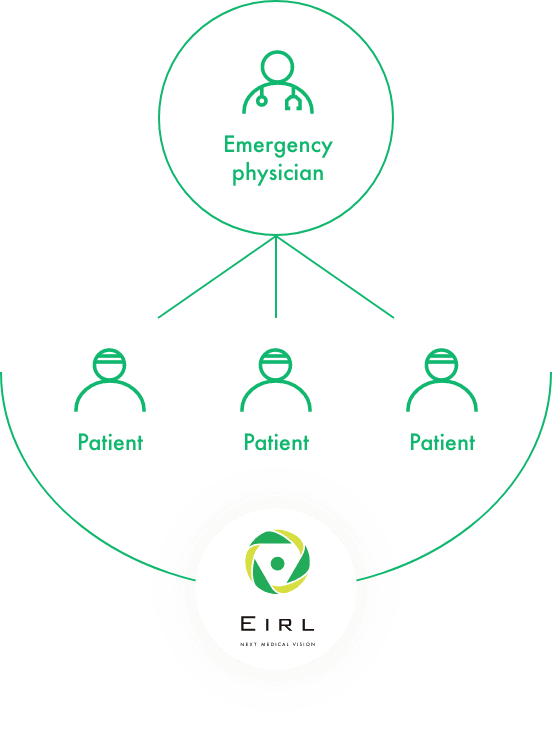
It has been pointed out that physicians at emergency department spend more time in the clinic and are on duty more often than those at other departments[4]. Thus, creating an environment supporting unskilled physicians is expected to reduce overused physicians in emergency departments.
Acknowledgements:
We would like to thank authors of SINet [5] for their work. Their work encouraged us to develop the software. We also appreciate the authors for the permission to use the codes for our medical products.[1]Medical facilities survey (static and dynamic), Overview of hospitals conducted by the Ministry of Health, Labour and Welfare, 2017 shows that facilities for emergency care in Japan consist of 288 primary, 4,006 secondary, and 1659 tertiary
[2]Ministry of Health, Labour and Welfare, Emergency Medicine and Current Issues
[3]Ministry of Health, Labour and Welfare, Current status of emergency centers and secondary emergency medical institutions
[4]as above
[5] Deng-Ping Fan, et al. Camouflaged Object Detection. CVPR 2020
Main features
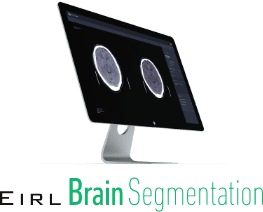
High attenuation areas in brain images extracted from CT images
High attenuation areas in brain images are extracted from the non-contrast head CT images and are highlighted. High attenuation areas in each slice will be displayed.
Basic Info
| Product Name | Medical Image Analysis Software, EIRL Brain Segmentation |
|---|---|
| Certification Number | 303AGBZX00043Z00 |
Requirements
| Modality | CT |
|---|---|
| Imaging Requirements | Axial、512×512pixel or above |
Integration Track Record
| Modality | CT |
|---|---|
| PACS | FUJIFILM Corporation, Nobori Ltd., Canon Medical Systems Corporation, Philips Japan, Ltd., PSP Corporation and other |
Frequently Asked Questions
How fast is the measurement speed per image?
After receiving images from PACS or modalities, it takes less than 60 seconds to send the result back to PACS.Once the storage in PACS is completed, you can check the result on your devices.
Can I see a demonstration?
We are in the middle of developing a trial version. We will contact you as soon as it is ready.